How Synthetic Data Transforms EHR and EMR Testing for FHIR Compliance and Healthcare QA
In today’s digitally connected healthcare landscape, Electronic Health Record (EHR) and Electronic Medical Record (EMR) systems are the backbone of patient data management. These systems support clinical workflows, billing, diagnostics, and data sharing across providers.
Healthcare organizations must test a wide array of workflows, from patient registration to billing, medication reconciliation, and lab result processing. Ensuring system integrity and interoperability across these domains demands high-quality, secure, and scenario-specific test data.
Historically, the industry has relied on masked production data, but this method falls short of delivering the flexibility, scale, and privacy assurance that modern systems require. Synthetic data is a secure, scalable and higher quality alternative for meeting the many test data challenges imposed by EHR/EMR testing.
The Evolving Landscape of Healthcare Interoperability
Interoperability is the cornerstone of modern healthcare IT strategy. Standards like HL7, FHIR, and X12 are designed to ensure that health data can be exchanged seamlessly between disparate systems. HL7 (Health Level 7) has been in use for decades, providing a messaging framework for clinical and administrative data. More recently, FHIR (Fast Healthcare Interoperability Resources), developed by HL7 International, has gained rapid adoption for its modern, API-based approach to data exchange using JSON and XML.
Several key factors are driving the shift toward FHIR and enhanced interoperability:
- The 21st Century Cures Act mandates that patients must have access to their health information via APIs, with FHIR as the standard of choice.
- CMS Interoperability and Patient Access Final Rule requires payers and providers to adopt FHIR APIs.
- A growing ecosystem of digital health apps, telemedicine platforms, and wearable devices requires standardized, on-demand data exchange.
- X12 is another key standard primarily used in claims, eligibility, and electronic remittance advice. X12’s structured format is vital for testing revenue cycle management systems and validating workflows between providers and payers.
Testing these standards presents unique challenges, including varying schema implementations, version mismatches, and intricate validation requirements.
Technical Challenges in Data Interoperability and Testing
EHR and EMR systems span a complex web of software modules, including patient registration, scheduling, billing, clinical documentation, lab results, and medication administration. Each module may rely on different standards and exchange data using a mix of HL7 messages, FHIR resources, and X12 transaction sets. Testing this ecosystem requires synthetic data that reflects real-world complexity while meeting strict compliance guidelines.
Technical hurdles in testing include:
- Validating interoperability and conformance to HL7, FHIR, and X12 across environments
- Generating consistent test data that respects referential integrity across patients, providers, encounters, and observations
- Simulating edge cases such as malformed HL7 messages, overlapping prescriptions, and claim denial loops
- Ensuring synthetic data aligns with evolving schemas and regulatory versions
- Integrating synthetic data generation into CI/CD pipelines for continuous testing
To meet stringent healthcare quality standards with agility and efficiency, test data must be 100% secure, aligned with test objectives, and delivered to automated testing as an integrated process at scale.
Limitations of Traditional Test Data Approaches
The conventional approach to healthcare application testing has involved copying production data and masking it to remove identifiable information. It’s an easy and familiar approach, but the risks and shortcomings are numerous:
- Masked data may still carry residual PHI or PII if poorly scrubbed
- Masked data fails to cover negative scenarios, edge cases, or rare conditions
- Manual data extraction and cleansing processes are time-intensive and error-prone
- Compliance with HIPAA, GDPR, and other privacy frameworks remains questionable
- There is little flexibility to scale masked data sets or simulate specific conditions for integration testing
As healthcare systems evolve to include more microservices, APIs, and cloud-based solutions, the limitations of traditional Test Data Management, based on static and cumbersome production test data sets, are becoming problematic for modern DevOps environments.
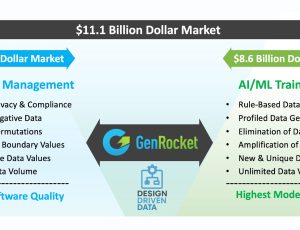
GenRocket’s Synthetic Data Solution: Design-Driven and Scalable
GenRocket provides a Design-Driven Synthetic Test Data platform that generates structured, compliant, and customizable data for literally every test scenario—without any reliance on sensitive production data.
The GenRocket paradigm enables organizations to dynamically create synthetic EHR/EMR datasets that simulate real-world complexity and business rules, with full referential integrity.
Key differentiators of GenRocket’s solution include:
- Metadata-driven generation: Data is generated based on XML schemas, relational database schemas, and HL7/FHIR/X12 metadata.
- Test case orchestration: The volume, variety, and format of generated synthetic data is designed to directly align with functional or performance test case objectives.
- Interoperability support: GenRocket offers generators for HL7 segments, FHIR resources, and X12 transactions.
- CI/CD integration: Data provisioning is automated through Jenkins, GitLab, Azure DevOps, and other dev and test automation tools.
- Scalability: Users can generate millions of records within minutes, enabling high-volume stress and integration testing.
Using GenRocket, organizations can transition away from slow, cumbersome, and insecure data provisioning toward an agile, automated, and secure test data strategy.
Strategic Benefits and Industry Adoption Trends
Synthetic data is gaining traction as a solution not just for compliance but also for innovation. Gartner predicts that by 2030, synthetic data will completely replace real data in AI model training environments. In healthcare, the value proposition is even stronger due to the sensitivity of patient data.
Adopting synthetic data for EHR and EMR testing delivers measurable ROI:
- Eliminates data privacy risks entirely
- Accelerates testing and reduces bottlenecks in QA
- Enhances test coverage and reliability of digital health platforms
- Supports AI-driven decision systems with statistically robust, unbiased training data
- Enables real-time validation of HL7/FHIR interfaces across partner systems and third-party apps
As interoperability standards evolve and more APIs are mandated, synthetic data enables organizations to test securely and without compromise.
A Diverse Data Landscape: HL7, FHIR and X12
Understanding the distinctions among healthcare interoperability standards is essential for successful data exchange and system testing. HL7, though widely adopted, has a fragmented implementation across organizations, with optional segments and custom fields that complicate integration and testing. It is text-based and relies on a pipe-delimited format, which limits its scalability in modern API ecosystems.
FHIR (Fast Healthcare Interoperability Resources) addresses these limitations with a modular, RESTful architecture using JSON and XML. It supports granular data access and interoperability across devices, applications, and systems. FHIR is also designed for mobile health (mHealth) and patient-facing apps, aligning with federal mandates for patient access and third-party API integrations. However, FHIR’s implementation maturity varies, and test data must account for incomplete resources and evolving profiles.
X12, in contrast, is entrenched in healthcare financial workflows. It defines structured formats for eligibility checks (270/271), claims submission (837), and remittance advice (835). Testing X12 processes requires validation of data fields, sequencing, acknowledgments, and rejection codes, all of which demand synthetic data that mimics payer-specific rules.
GenRocket supports all of these standards with a flexible architecture that can adapt to any data requirement for any testing or training environment.
Regulatory and Compliance Imperatives
Regulatory requirements are becoming increasingly prescriptive about data access, patient rights, and testing rigor. The Office of the National Coordinator (ONC) mandates that certified health IT developers support standardized APIs using FHIR under the 21st Century Cures Act. The Centers for Medicare & Medicaid Services (CMS) enforce penalties for non-compliance with API access rules. Meanwhile, HIPAA, GDPR, and CCPA continue to impose severe restrictions on the use of identifiable health data in non-production environments, prompting healthcare organizations to seek alternative approaches that maintain compliance while enabling agile development and testing.
For healthcare organizations, this creates a dual mandate: safeguard patient data while accelerating digital innovation. Synthetic test data provides the dual benefit of removing real data from lower environments while enabling robust, standards-based testing across multiple workflows.
Future Outlook: AI, Personalization, and Data Simulation
As AI and machine learning become embedded in healthcare delivery, the need for high-quality, synthetic training and testing data will expand exponentially. Algorithms supporting early diagnosis, risk prediction, care coordination, and fraud detection depend on data sets that reflect clinical diversity, eliminate statistical bias, and include edge cases. Synthetic data can be engineered to represent all these attributes while maintaining compliance.
Synthetic data will also be critical in precision medicine, where personalized health records, genomics, and social determinants of health must be tested across massive combinations of variables.
GenRocket’s platform can be leveraged not only for software QA, but also for simulating clinical workflows, generating variant-rich datasets, and stress-testing algorithmic behavior under real-world conditions when training machine learning models.
Key Takeaways
The healthcare industry stands at a pivotal moment where interoperability, security, and innovation intersect. Standards like FHIR, HL7, and X12 are reshaping the landscape—but testing these systems with legacy data tools puts organizations at risk of noncompliance and operational failure.
GenRocket’s synthetic data generation platform equips healthcare organizations with the power to provision, control, and scale synthetic test data for every use case—whether validating an API, simulating millions of claims, or training a machine learning model. With regulatory mandates intensifying and digital transformation accelerating, synthetic data isn’t just a nice-to-have—it’s a strategic imperative.